Jeremy Towns, MD; Christopher N. White, MD
Department of Emergency Medicine, University of Alabama at Birmingham, Birmingham, AL
Abstract
A 32-year-old male with a history of recently diagnosed diabetes, hyperlipidemia and hypertension presented to our emergency department due to right sided headache associated with hiccups, dizziness, imbalance, right facial, left arm and left leg “sleepiness”. The patient also complained of vertiginous symptoms that worsened with head position. CT angiography of the head and neck were obtained and revealed a high-grade stenosis of the intracranial right vertebral artery, short segment, with occlusion, secondary to dissection. Inpatient MRI showed a subacute right lateral medullary infarction (Wallenberg Syndrome).
Introduction
The incidence of vertebral artery dissection (VAD) is estimated to be 1 in 100,000. VAD only accounts for 2 in 100 ischemic strokes. However, it is an important cause of stroke in young adults. Marfan syndrome and Ehlers-Danlos are two known connective tissue malformations that may increase the risk of VAD. However, other unnamed disorders may also be implicated. VAD incidence seems to have increased over time and is thought to be related more to the improvement in imaging technology. Dizziness/vertigo is the most commonly reported symptom associated with VAD. VAD can also lead to lateral medullary syndrome, posterior circulation syndromes or cervical spinal cord ischemia.
Lateral medullary syndrome is the most common and important syndrome related to intracranial vertebral artery occlusions and have a number of important diagnostic features. Vestibulocerebellar symptoms that result in dizziness and imbalance are universally present. Additionally, nystagmus is nearly always present. Nystagmus can have both horizontal and rotational components. Ipsilateral facial as well as contralateral trunk and extremity sensory symptoms, such as pain and temperature loss, are common. Bulbar muscle weakness may result in hoarseness, dysphagia, aspiration, dysarthria, dysphonia and hiccups.
Inpatient MRI showed a subacute right lateral medullary infarction (Wallenburg Syndrome). He was started on aspirin therapy in addition to his home medications and provided stroke risk education.

Severe short segment of the right V4 segment of the right vertebral artery with near occlusion
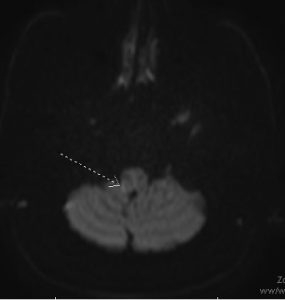
Subtle questionable restricted diffusion in the posterolateral right medullar with associated T2/FLAIR hyperintense signal suspicious for a small infarct
Discussion
We present a case of a missed vertebral artery dissection resulting in neurological deficits indicative of lateral medullary syndrome in a young adult. VADs can be easily missed on first presentation to the emergency department, especially in young patients. 13 percent of cases of ischemic stroke in VAD occur after a previous TIA. Vertebral artery dissections are most likely to occur in segments V2 and V3, with V1 and V4 less likely. Non-contrasted CT imaging of the head is likely to miss this diagnosis. Use of multimodal CT or MR imaging is crucial to identifying vessel abnormalities and making the diagnosis. High Resolution Magnetic Resonance can be deployed when other imaging is inconclusive as sometimes the venous plexus may be mistaken for a VAD. Studies have not shown that antithrombotic therapy is superior to antiplatelet therapy. VADs heal on average within 6 months. In conclusion, it is vitally important to perform a thorough physical examination, recognize classic patterns/syndromes associated with specific neuroanatomical injury, and obtain appropriate advanced imaging before closing the diagnostic loop.
References
- Arnold, Marcel, et al. “Vertebral artery dissection: presenting findings and predictors of outcome.” Stroke 37.10 (2006): 2499-2503.Espinosa G, Bucciarelli S, Cervera R, Gómez-Puerta JA, Font J. Laboratory studies on pathophysiology of the catastrophic antiphospholipid syndrome. Autoimmunity Reviews. 2006;6(2):68-71.
- Dunay SN, Perreault MD, Grubish LK. A Case of Delayed Traumatic Vertebral Artery Dissection. Mil Med. 2018 May 1;183(5-6):e276-e277. doi: 10.1093/milmed/usx096. PMID: 29415135.
- O. Naggara, F. Louillet, E. Touzé, D. Roy, X. Leclerc, J.-L. Mas, J.-P. Pruvo, J.-F. Meder, C. Oppenheim American Journal of Neuroradiology Oct 2010, 31 (9) 1707-1712; DOI: 10.3174/ajnr.A2165
- Redekop G J: Extracranial carotid and vertebral artery dissection: a review. Can J Neurol Sci 2008; 35(2): 146–52.
