David Pigott MD RDMS FACEP
Mathew Neth MD
UAB Department of Emergency Medicine
Division of Emergency Ultrasound
Case
This 39-year-old male with a history of HTN, polycystic kidney disease presented with chest pain and syncope while eating dinner at a bar. He was transported by helicopter to the emergency department with concern for acute MI.
In the emergency department, an EKG showed nonspecific ST-T wave changes, d-dimer 288, troponin 0.02 (normal <0.04) and chest x-ray was unremarkable.
Although the initial plan was to admit for CP rule-out, the patient dropped his pressure to the 70s while still in the emergency department. A bedside ultrasound was performed.
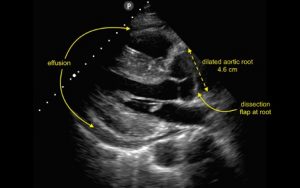
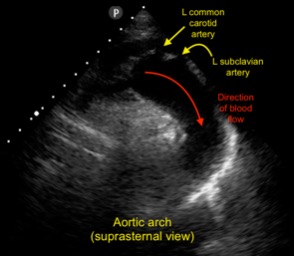
The bedside ultrasound showed a large pericardial effusion with mixed blood and clot as well as a markedly dilated aortic root (normal <4 cm). Close examination of the aortic root revealed the presence of a dissection flap just distal to the valve leaflets. A large mobile clot is seen within the pericardium (motion images not available for this publication). A suprasternal view of the aortic arch did not show further dissection within the arch.
The patient was taken emergently to the OR by CV Surgery where a proximal aortic dissection (Stanford A) was found and repaired as well as hemopericardium with tamponade.
Copyright permission has been obtained from the UAB Department of Emergency Medicine Division of Ultrasound, Dr. David C. Pigott MD Co-Director of UAB EM Emergency Ultrasound
