David Pigott MD RDMS FACEP
Keegan Nicodemus MD
Stephen Knight MD
UAB Department of Emergency Medicine
Division of Emergency Ultrasound
Case Presentation
62-year-old male with a history of CAD status post CABG 4 weeks prior, HTN, HLD, DM2, HCV, who presents with 3 days of worsening shortness of breath. While en route to ED, he had a severe coughing episode where he felt his sternum move/shift and acute chest pain.
On exam, the patient was afebrile with normal blood pressure, with HR 125, RR 25. Oxygen saturation was 97% on RA. On exam, a 3 cm ecchymosis was noted over the inferior portion of the sternal incision site.
Point-of-care ultrasound (POCUS) was performed:
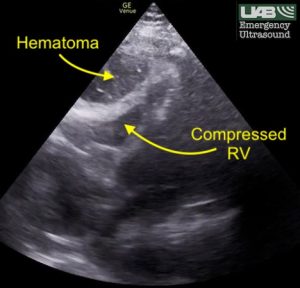
Findings included a normal left ventricular ejection fraction and a collapsible IVC with bilateral B-lines. Also noted was a large anterior hematoma which appeared to be causing extrinsic compression of the right ventricle.
Because of the concern for preload dependence, IV fluid was started and cardiovascular (CV) surgery was consulted. CT chest with contrast was obtained.
CT angiography of the chest demonstrated obvious sternal dehiscence with a large retrosternal hematoma causing compression of the right ventricle and proximal pulmonary trunk. A moderate left pleural effusion with atelectasis was also noted.
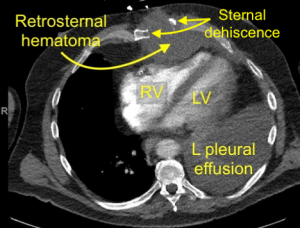
The patient was taken emergently to the OR for evacuation of the retrosternal hematoma and rewiring of sternal dehiscence. Upon surgical decompression of the hematoma in the OR, the patient’s hemodynamics markedly improved. The patient required 2 units PRBC transfusion in the OR.
The patient is still hospitalized but is recovering well.
Discussion
Typically, pericardial tamponade is caused by compression of the right ventricle by fluid or blood within the pericardial space, leading to an obstructive shock picture. In this case, a process known as extrapericardial tamponade was likely the culprit. Although the patient did not have severely altered hemodynamics, compression of the right ventricle by the retrosternal hematoma noted on POCUS and again on CT was clearly responsible for the patient’s presentation, as well as the patient’s rapid improvement following surgical decompression.
The presence of a mediastinal hematoma has been implicated in the development of extrapericardial tamponade and may occur from multiple causes, including blunt chest trauma, aneurysmal rupture of the aorta or carotid artery, or penetrating mediastinal or cardiac injury.
Rodgers-Fischl PM, Makdisi G, Keshavamurthy S. Extrapericardial Tamponade After Blunt Trauma. Ann Thorac Surg. 2021 Jan;111(1):e49-e50.
Sabatel-Perez F, Sastre-Perona MA, Alonso MB, Rodríguez Padial L. Extrapericardial cardiac tamponade due to massive retrosternal hematoma. Cardiol J. 2019;26(5):616-617.
Copyright permission has been obtained from the UAB Department of Emergency Medicine Division of Ultrasound, Dr. David C. Pigott MD Co-Director of UAB EM Emergency Ultrasound
