Benjamin von Schweinitz MD, Christopher Greene MD, James Booth MD
UAB Department of Emergency Medicine
Introduction
After a cohort of patients who presented with influenza-like illness in Wuhan, China that led to the discovery of a novel coronavirus, COVID-19, there have been many alterations in clinical practice due to the virus’s increased virulence and transmission. In-Vivo and clinical research has determined that most of the transmission of the virus comes from airborne droplets. (1) In the hospital setting intubation, noninvasive ventilation, and nebulization of medications carry the highest droplet generating potential, and throughout the outbreak personal protective equipment, PPE, has been directed preferentially to providers performing these procedures. (2,3) Medical professionals are faced with the challenge of trying to help patient suffering from COVID-19 but also protecting themselves and other patients from spread. The delivery of advanced cardiac life support has posed a unique challenge to the healthcare system. The following article will discuss our hospital’s multidisciplinary approach of the management of patients during cardiac arrest.
Staffing
Our hospitals like many others were faced with challenges of how to deliver advanced cardiac life support in the new confines of limited medical resources. Prior to COVID-19 infections our delivery of arrest and post-arrest care included a large multidisciplinary team of doctors, nurses, respiratory therapist, and pharmacists. However, concerned that cardiac arrest care carries a high degree of transmission risk to healthcare workers, we distilled this team down to minimize healthcare exposure while maintaining a high degree of medical capability for the patient. Below is a figurative diagram of healthcare workers with associated roles and responsibilities.
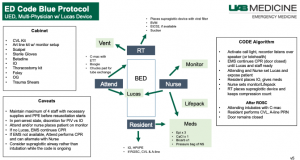
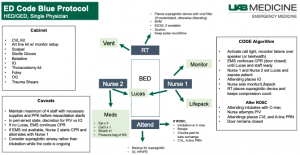
In this diagram we have reduced the number of healthcare workers engaged and advanced cardiac life support at the bedside while separating other healthcare workers outside the room. This creates a cold (lower risk of exposure) and warm (higher risk of exposure) zone similar to precautions taken during healthcare delivery of patients exposed to chemical or biology agents.(4) Prior to the pandemic we had limited, but large and well-stocked caches of supplies at various high utilization areas throughout the emergency department. A “runner” would be able to get a needed supply quickly for the resuscitation team if needed. In the setting of a pandemic, we found that this type of approach promoted breaks in containment and PPE, and increased the risk of exposure to staff in the cold zones. To mitigate this risk, we devised a list seen in this figure of essential supplies that would allow the practitioners in the room to deliver cart cardiac arrest care into post-arrest care, and stocked a mobile cart which could be wheeled outside the resuscitation room to promote batching of supply introductions.
Airway Management
Prior to the pandemic, our overall physician practice pattern was to perform endotracheal intubation on cardiac arrest patients. Since COVID, we have increased our unitization of supraglottic devices such as LMA’s and iGels. If return of spontaneous circulation is obtained, then the physician would perform endotracheal intubation after ROSC.(3) We discouraged bag-valve-mask ventilation due to its incomplete seal that potentially would allow for more aerosolization of the viral particles. To date we cannot find any literature that supports or disproves the comparison of supraglottic devices to endotracheal tubes as it relates to aerosolization. There is evidence to suggest that the use of viral filters on the ventilatory machines as well as bag valve mask capture virologist smallest 5 µm thus limiting risk to medical staff. (6)
Personal Protective equipment
Another challenge in implementing this new model has been the donning of personal protective equipment prior to engagement and BLS or ACLS. As healthcare professionals we have a calling or desire to want to rapidly respond to someone in distress. Due to concerns about widespread transmission among hospital staff compromising the available workforce, we have instructed staff to don personal protective equipment prior to engagement in CPR. Our hospital has chosen to use N-95 mask and full face shield. This in theory will help prevent the virus from coming into contact with nasopharyngeal and ocular membranes. Also, there is a requirement for impermeable gown and double gloves during the delivery of ACLS. This is to reduce the person-to-person transmission for the health and safety of other patients. We had designated a quality control individual, usually nursing, whose role and responsibility and codes is to monitor for compliance and assist donning and doffing procedures.
Negative pressure or HEPA filter rooms
We have been fortunate in our Emergency Department that to acquire large HEPA filter devices that have the ability to transform a number of our rooms into substitutes to our 4 negative pressure rooms. These rooms solely for high risk aerosolization procedures and cardiac arrest. If ROSC we then move the patient to a regular room. The negative pressure room is then left undisturbed for one hour prior to disinfection and reuse. Prior to the pandemic we had an endless supply of resources that we could pull from other parts of the emergency department in order to care for patient. However, we found that this was not an efficient method of allowing for multiple breaks in the negative pressure system therefore we devised a list seen in this figure of essential supplies that would allow the practitioners in the room to deliver cart cardiac arrest care into post-arrest care.
Automatic compression devices
Prior to the pandemic arm main source for closed cardiac compression was the use of available manpower. This included nursing, nursing assistants, patient care techs, and trainees.
Through simulation we found quickly that in a limited staffing model for the delivery of cardiac arrest care that it was not sustainable to deliver high-quality compressions and full protective personal equipment requirements. This led to the rapid acquisition and purchase of external compression devices. While no data shows that these devices are superior to human delivered compressions they have been able to be beneficial in the limitations of delivering CPR and a resource limiting setting.
Conclusion
While we have limited the hospital personnel contact with a patient during ACLS, the above model as allowed for continued delivery of essential interventions during cardiac arrest. Given community spread, it has been difficult to determine if the above as reduced transmission to healthcare professionals our contact tracing has not found an individual become infected with COVID after ACLS delivery using the above system.
References
- Jayaweera M, Perera H, Gunawardana B, Manatunge J. Transmission of COVID-19 virus by droplets and aerosols: A critical review on the unresolved dichotomy. Environ Res. 2020;188:109819. doi:10.1016/j.envres.2020.109819Tran K
- Cimon K, et al. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012; 7e35797
- Davies A, Thomson G, Walker J, Bennett A (2009) A review of the risks and disease transmission associated with aerosol generating medical procedures. Journal of Infection Prevention 10: 122–126
- Razak S, Hignett S, Barnes J. Emergency Department Response to Chemical, Biological, Radiological, Nuclear, and Explosive Events: A Systematic Review. Prehosp Disaster Med. 2018 Oct;33(5):543-549. doi: 10.1017/S1049023X18000900. PMID: 30379127.
- Panchal AR, Berg KM, Hirsch KG, Kudenchuk PJ, Del Rios M, Cabañas JG, Link MS, Kurz MC, Chan PS, Morley PT, Hazinski MF, Donnino MW. 2019 American Heart Association Focused Update on Advanced Cardiovascular Life Support: Use of Advanced Airways, Vasopressors, and Extracorporeal Cardiopulmonary Resuscitation During Cardiac Arrest: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2019 Dec 10;140(24):e881-e894. doi: 10.1161/CIR.0000000000000732. Epub 2019 Nov 14. PMID: 31722552.
- World Health Organization. (2020). Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations: scientific brief, 29 March 2020. World Health Organization. https://apps.who.int/iris/handle/10665/331616. License: CC BY-NC-SA 3.0 IGO
