Kevin S. Barlotta, MD
Joseph Cortopassi, MD
University of Alabama at Birmingham (UAB)
Chief Complaint: Altered mental status
HPI: 35-year-old male with a history of intravenous drug abuse (IVDA) presenting the emergency department via EMS from home after family called reporting patient was unresponsive. EMS described a patient lying across a bed with spontaneous respirations and palpable pulses. The patient was placed on supplemental oxygen and IV access was obtained. The patient was euglycemic and failed to respond to IV Narcan administration. In route, the patient became combative and was noted to be moving only his upper extremities. He received ketamine for sedation and was unable to provide additional history upon arrival. Family was not available.
Physical Exam: 122/79 66 22 97.4 96% RA
- General: Alert, spontaneously breathing with patent airway and occasional moaning. Patient noted to move upper extremities (UE) without movement of his lower extremities (LE). No obvious signs of trauma. Peripheral pulses intact.
- HEENT: No signs of trauma. PERRL with disconjugate gaze, sclera anicteric. Oropharynx clear.
- Neuro: GCS 8. Spontaneous non-purposeful movement of the UE with painful withdrawal on exam. No response to pain in bilateral LE. Incomprehensible verbal sounds. Eye opening to pain.
- Back and cervical spine: No midline tenderness obvious on exam. No step-offs or external signs of trauma. No decubitus ulcer or skin changes. No surgical scars.
- Extremities/Skin: No gross deformities, pressure-like skin changes right malleoli. Soft compartments.
ED Course:
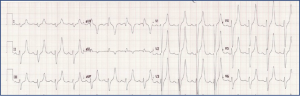
- Patient placed on cardiac monitor and supplemental oxygen. A point of care glucose (270 mg/dL) and lack of response to Narcan were confirmed. Intravenous fluids were administered and preparation for airway management were arranged. A STAT neurosurgical consultation was placed to aid in bedside assessment prior to intubation. An electrocardiogram was obtained (figure 1).
Figure 1: Electrocardiogram 1
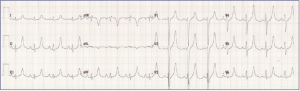
Following EKG interpretation, the patient was treated with additional IV fluids, calcium gluconate, sodium bicarbonate and dextrose/insulin therapy. Renal and medical intensive care unit (MICU) consults were placed. The patient was intubated without complication and a second EKG was obtained (figure 2).
Figure 2: Electrocardiogram 2
- Initial laboratory studies reveal acute kidney injury with a BUN of 36 mg/dL, a creatinine of 4.3 mg/dL and a GFR of 16 mL/min/1.73m2.
- A non-hemolyzed serum potassium was elevated at 8.9 mmol/L.
- A serum glucose of 277 mg/dL was obtained with note of a high-anion gap (26) and serum bicarbonate level of 12 mEq/L. Transaminase levels were elevated (AST 3461 Units/L, ALT 1785 Units/L) and a serum creatinine kinase was > 100,000 Units/L (after several attempts to dilute the sample).
- A serum white blood cell count (WBC) of 35.3 cm3, lactic acid of 5.9 mmol/L and ESR of 9 mm/hr were obtained.
- Following intubation an orogastric tube and Foley catheter were inserted (figure 3). A urinalysis revealed 3+ protein and blood with 3 red blood cells (RBC).
- A urine drug screen was positive for amphetamines and fentanyl.
- A covid-19 PCR was negative/not detected.
Figure 3: Foley catheter: Urine output

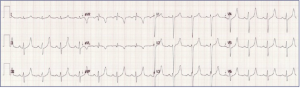
- Continuous IV fluids combined with repeat doses of IV calcium and dextrose/insulin therapy were effective in lowering the serum potassium levels (6.4 mEq/L after first 4 hours). A third EKG was obtained (figure 4).
Figure 4: EKG 3
- Advanced imaging did not reveal a spinal cord lesion or insult. An MRI of the lumbar spine noted diffuse grade 1 atrophy of the lumbar paraspinal muscles. The patient was ultimately admitted to the MICU for continuous renal replacement therapy (CRRT) and medical management.
Discussion:
Rhabdomyolysis is a serious medical condition characterized by the breakdown of skeletal muscle tissue and release of intracellular contents into the blood stream. Rhabdomyolysis can lead to acute kidney injury (AKI) and is a potentially life-threatening condition. This is a case of rhabdomyolysis with myoglobinuric renal failure and hyperkalemia due to toxic myopathy secondary to drug overdose and prolonged downtime. Our patient presented with altered mental status complicated by personal IVDA and EMS administration of ketamine. Exclusion of immediate, reversible causes of altered mental status (POC-glucose and Narcan administration) were confirmed and the patient was intubated for both airway protection and facilitation of assessment. An EKG concerning for hyperkalemia (peaked T-waves and a prolonged QRS complex) was obtained, prompting initiation of early empiric treatment and consultation with nephrology to initiate dialysis. Although secondary survey revealed what appeared to be a spinal cord insult, the patient’s lower extremity weakness was attributed to a toxic myopathy and neuropathy resulting from rhabdomyolysis and a prolonged downtime following an opioid overdose (heroin and fentanyl). Dialysis was discontinued on hospital day eighteen and the patient was ultimately discharged on hospital day twenty-four with home health services and physical therapy. Addiction medicine was consulted to assist in addressing the patient’s substance abuse disorder.
Toxic myopathies are a very well-known phenomenon in medicine and can be classified into multiple subcategories based on pathogenic mechanisms. Muscle tissue is very sensitive to many different substances including alcohol, common pharmaceutical drugs such as statins, rheumatological drugs, steroids etc., and in rarer circumstances, illicit drugs such as amphetamines and other stimulants. Diagnosis is imperative on early identification and a thorough medication or drug history. Early recognition is important because the vast majority are reversible if end organ damage can be prevented. Recovery varies based on severity, but as in our case, typically takes several weeks to months. Given its association with rhabdomyolysis, renal injury is a common finding and in severe cases renal replacement therapy is warranted.
STAT review: Hyperkalemia on EKG
Peaked T-waves
Prolonged PR interval
Loss of P waves
Prolonged QRS
ST-segment elevation
Ectopy & escape
Progressive QRS widening
Sine wave
Ventricular fibrillation
Asystole
- Rafique Z, Peacock F et al. Hyperkalemia management in the emergency department: An expert panel consensus. J Am Coll Emerg Physicians Open 2021 Oct; 2(5): e12572.
- Long B, Koyfman A, Gottlieb M. An evidence-based narrative review of the emergency department evaluation and management of rhabdomyolysis. Am J Emerg Med. 2019 Mar;37(3):518-523
- Pasnoor M, Barohn RJ, Dimachkie MM. Toxic myopathies. Neurol Clin. 2014;32(3):647-viii. doi:10.1016/j.ncl.2014.04.009
