William Rushton; Jessica Rivera
Alabama Poison Information Center, Children’s of Alabama
Office of Medical Toxicology, University of Alabama Birmingham
Background
Hydroxocobalamin is an FDA approved drug for the treatment of cyanide toxicity. Adult dosing usually requires 5gms run over 15 mins for suspected toxicity, binding cyanide, and forming nontoxic cyanocobalamin, otherwise known as B12. Phase 1 trials of hydroxocobalamin, however, showed an interesting side effect. In addition to the commonly described reddish discoloration to the urine and the skin, healthy volunteers in the study experienced transient increases of blood pressure that would take up to 4 hours to return back to baseline [1]. Subsequent studies were notable for a unique finding with hydroxocobalamin: in addition to binding cyanide, it could also act as a scavenger for nitric oxide, an important second messenger involved in arterial dilation [2].
Recently, there has been increased attention on using hydroxocobalamin’s nitric oxide (NO) scavenging ability for other types of refractory shock [3]. For instance, cardiac arrest due to hypothermia can be a challenging to treat particularly as warming measures may initially prove to be ineffective. Yet, standard teaching argues against ceasing cardiopulmonary resuscitation (CPR) until normothermia has been obtained. We present a case of hypothermic induced cardiac arrest and resultant shock that eventually demonstrated improvement in hemodynamics and core body temperature following rescue therapy with hydroxocobalamin.
Case
A 40 year-old male with a history of HIV presented to a Birmingham, AL emergency department in full cardiac arrest. History obtained later confirmed that the patient was abusing heroin and ethanol before becoming unconscious outside where the environmental temperature was 27 Celsius. Initial rhythm was pulseless electrical activity (PEA) and initial core body temperature was 29 Celsius.
Epinephrine, calcium, naloxone, and sodium bicarbonate therapy were administered and return of spontaneous circulation was obtained after 10 minutes of CPR; osborn waves were subsequently visualized on electrocardiogram (EKG). He was started on maximum dose of epinephrine, norepinephrine, phenylephrine, and vasopressin infusions as well was warm water gastric lavage and application of a non-invasive targeted temperature management device. These therapies were unable to increase systolic blood pressure (SBP) greater than 50mmHg and core body temperature remained less than 30 Celsius.
Five grams of hydroxocobalamin was bolused with immediate temporal improvement of SBP to 190mmHg and temperature to 33 Celsius. Vasopressin and phenylephrine were discontinued while epinephrine and norepinephrine infusions were rapidly titrated down. He sustained rapid improvement of hemodynamics and became normothermic over the next 36 hours but was ultimately removed from ventilator support secondary to severe anoxic injury seen on neuroimaging.

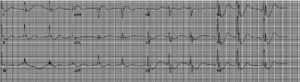
Figure 1: EKG following return of spontaneous circulation with prominent Osborn waves.
Discussion
This case demonstrates a patient with severe refractory shock and hypothermia that did not respond to aggressive external and internal cooling measures with concurrent maximum vasopressor therapy until a dramatic and temporal improvement was noted after treatment of hydroxocobalamin. In severe hypothermia, cardiovascular collapse occurs largely to impediment of ion currents during all stages of the cardiac action potential. At the same time, systemic vascular resistance falls with severe hypothermia as catecholamine release is blunted, a process similar to vasoplegia pathophysiology [4].
Recently, hydroxocobalamin has been the focus of much investigation for mechanisms independent of its role in treating cyanide poisoning and ex vivo models have focused on its ability to scavenger nitric oxide (NO) and to potentially inhibit nitric oxide synthase, thereby decreasing endogenous NO and increasing systemic vascular resistance. Based on these investigations, several case reports have also focused on hydroxocobalamin’s role in vasoplegic syndrome with similar temporal improvement in patients’ hemodynamics [4,5]. Another recent case report also reported successful improvement in hemodynamics in a patient with septic shock [1]. However, optimal dosing remains ambiguous and evidence-based trials are lacking in human populations.
Hydroxocobalamin could be considered in refractory hypothermic shock to increase systemic vascular resistance and to potentially increase efficacy of warming measures. Further high evidence-based research is needed. Hydroxocobalamin is not FDA approved in treating shock not related to cyanide
toxicity; however, alternatives to use can be discussed physician experts at the Alabama Poison Information Center (1-800-222-1222).
Reference/Further Reading:
- Uhl W, Nolting A, Golor G, Rost KL, Kovar A. Safety of hydroxocobalamin in healthy volunteers in a randomized, placebo-controlled study. Clin Toxicol (Phila). 2006;44 Suppl 1:17-28. doi:10.1080/15563650600811755
- Gerth K, Ehring T, Braendle M, Schelling P. Nitric oxide scavenging by hydroxocobalamin may account for its hemodynamic profile. Clin Toxicol (Phila). 2006;44 Suppl 1:29-36. doi:10.1080/15563650600811805
- Carullo PC, Al-Khafaji A. Hydroxocobalamin in the treatment of vasodilatory shock. J Clin Anesth. 2020;61:109665. doi:10.1016/j.jclinane.2019.109665
- Cai Y, Mack A, Ladlie BL, Martin AK. The use of intravenous hydroxocobalamin as a rescue in methylene blue-resistant vasoplegic syndrome in cardiac surgery. Annals of cardiac anaesthesia. 2017 Oct;20(4):462.
- Weinberg JB, Chen Y, Jiang N, Beasley BE, Salerno JC, Ghosh DK. Inhibition of nitric oxide synthase by cobalamins and cobinamides. Free Radical Biology and Medicine. 2009 Jun 15;46(12):1626-32.
