Pasquale M, Sochovka Johnson E, Coan Farmer K, Rivera J, Green Vance E
Department of Pharmacy, UAB Hospital, Birmingham, Alabama
The practice of using push-dose or bolus vasopressors (also known as push-dose pressors and will be referred to as PDP or PDPs) has sparked a great deal of commentary in the FOAMEd (Free Open Access Medical Education) and traditional literature environments. As the practice of preparing appropriate concentrations of PDP medications is considered very high risk for error for a multitude of reasons, the authors summarize appropriate use of PDPs and what we feel are best practices for use and preparation of PDPs.
PDPs are most frequently used in the emergency department for hypotension with a high shock index in the peri-intubation setting, when return of spontaneous circulation occurs following cardiac arrest, and when there is a delay in obtaining and/or initiating a vasopressor for a hypotensive patient.
The two most well studied PDPs in the emergency department include phenylephrine and epinephrine. Phenylephrine acts as a pure alpha-1 receptor agonist, which could be beneficial for patients with hypotension and tachycardia since beta adrenergic agonism is avoided.(1) Phenylephrine as a PDP is dosed at 50 – 200 mcg every 2-5 minutes as needed. One notable side effect of phenylephrine is bradycardia as a result of peripheral vasoconstriction. Epinephrine has both alpha-1 receptor activity as well as beta-1 and -2 activity, which could be beneficial for patients with both hypotension and bradycardia. Epinephrine as a PDP is dosed at 5 – 20 mcg every 2 – 5 minutes as needed.1 Epinephrine has the potential to cause tachycardia due to its agonism of beta-adrenergic receptors. Both medications have data supporting their efficacy, with phenylephrine increasing systolic blood pressure (SBP) by a median of 20 mm Hg in one study; epinephrine was found in another study to increase SBP by a median of 13 mm Hg.(2,3)
While PDP use could certainly be beneficial for patients experiencing transient hypotension, it should be noted that these medications are not benign and have the potential to cause detrimental side effects. Additionally, the preparation and dilution of these medications in emergent situations could lead to significant dosing and/or administration errors. One study that examined the use of push dose phenylephrine and ephedrine found that 17 patients experienced an SBP increase > 100% or heart rate increase > 30%, with 12 patients receiving over the maximum recommended dose of phenylephrine of 200 mcg.(4) Another study published earlier this year found significant errors in documentation, preparation, and administration of PDPs. In this study, multiple dilution and administration errors were reported – some notable adverse events included extreme tachycardia (> 140 beats per minute), hypertension (SBP > 160 mm Hg), and ventricular tachycardia.(5) In some instances, patients received 10-fold or 100-fold overdoses. Based on this information, thorough knowledge in the dosing, preparation, and administration of these medications is vital for patient safety.
Phenylephrine and epinephrine prefilled 10 mL syringes are available for purchase from various manufacturers in the concentrations of 40 mcg/mL (400 mcg/10 mL) and 10 mcg/mL (100 mcg/10 mL), respectively. The advantages of stocking and using these in the ED are that they do not require dilution or preparation, and preclude math errors that may be made in a high-stress situation. The disadvantages include relatively infrequent use, high cost, and short expiration dating. However, best practice to reduce safety risks associated with dilution/admixing errors is to stock these prefilled syringes in the automated dispensing cabinets (ADCs) in the ED so that they are readily available. The authors recommend that only a licensed independent provider that is very familiar with PDP dosing and potential adverse effects administer these medications.
If stocking prefilled PDP syringes in your ED’s ADC is not feasible, PDP epinephrine may be prepared by withdrawing the contents of a 1 mg/1 mL epinephrine vial (formerly known as a 1:1000 concentration), adding this to a 100 mL normal saline bag, and withdrawing the contents into a syringe or syringes that have been labeled as containing epinephrine 10 mcg/mL. Some sources recommend using a “code” syringe of epinephrine (1 mg/10 mL), removing 1 mL from a normal saline flush, and inserting a needle through the tip of the flush to inject 1 mL (100 mcg) of epinephrine for a resulting concentration of 10 mcg/mL.(6) The authors of this publication do not recommend this practice due to the difficulty in accurately measuring 1 mL of epinephrine from a 10 mL syringe due to the air bubble present, and the difficulty in using a needle to inject through the tip of a saline flush (some of the authors have experienced either flush or epinephrine squirting out of the tip, resulting in an unknown concentration). Additionally, the Institute for Safe Medication Practices recommends against dilution of medications in flushes as these devices have been approved for flushing of vascular access devices, not for dilution and subsequent administration of IV push medications.(7) Phenylephrine vials are available as 10 mg/mL. Phenylephrine 10 mg may be added to a 100 mL normal saline bag for a resulting concentration of 100 mcg/mL. Please note that this is more concentrated than the 40 mcg/mL prefilled syringes. When these medications are prepared/diluted by care team personnel, it is imperative they are labeled appropriately with the drug name, prepared (resulting) concentration, time of preparation, and expiration time (dilutions prepared outside of a sterile hood must be used within one hour from the start of preparation; any remaining medication must be discarded after that time).(8)

Image from: https://www.mountainside-medical.com/products/adrenalin-epinephrine-injection-1mg-1-1000-vial-1-each
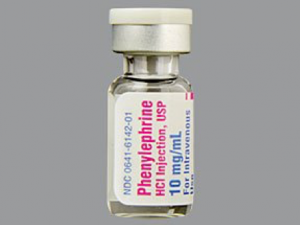
Image from: https://www.webmd.com/drugs/2/drug-12000/phenylephrine-injection/details

Image from: https://www.bbraunusa.com/en/products/b1/0-9-sodium-chlorideinjectionusp100mlfillin150mlpab.html
If you have a pharmacist member of the care team in your ED, this is the ideal team member to prepare PDPs. We do not recommend the provider leading the team prepare PDPs as this will add to the already heavy cognitive load of caring for a critically ill patient.
References:
- Tilton, et al. Utility of push-dose vasopressors for temporary treatment of hypotension in the emergency department. J Emerg Nurs. 2016 May;42(3):279-81
- Schwartz, et al. The impact of push-dose phenylephrine use on subsequent preload expansion in the ED setting. Am J Emerg Med. 2016 Dec; 34(12):2419-2422.
- Nawrocki, et al. Push Dose Epinephrine Use in the Management of Hypotension During Critical Care Transport. Prehosp EmergCare. 2019 Feb 26:1-8.
- Rotando A, et al. Push dose pressors: experience in critically ill patients outside of the operating room. Am Jour Emerg Med. 2019;494-498
- Cole J, et al. Human errors and adverse hemodynamic events related to “push dose pressors” in the emergency department. J Med Toxicol. 2019 Jul 3.
- EMCrit Push Dose Pressors. From: http://emcrit.org/wp-content/uploads/push-dose-pressors.pdf
- ISMP Safe Practice Guidelines for Adult IV Push Medications. From: https://www.ismp.org/sites/default/files/attachments/2017-11/ISMP97-Guidelines-071415-3.%20FINAL.pdf
- What is the immediate-use provision in USP <797>? From: http://www.snmmi.org/IssuesAdvocacy/content.aspx?ItemNumber=4907
