Brown, J MD; Smith A MD; Arnold J MD, Rushton W MD
Department of Emergency Medicine
UAB School of Medicine
Case
A 25-year-old female presented to the emergency department complaining of shortness of breath for 24 hours. Her dermatologist had prescribed Dapsone three times a day for dermatitis herpetiformis 36 hours ago. She reported ingesting three doses and subsequently became short of breath at rest and with exertion. Her presentation was notable for “purple lips,” palpitations, headache, and presyncope.
Upon arrival, she was hypoxic on room air at 88% SpO2 and tachycardic with a heart rate of 105 beats per minute. Physical exam revealed perioral cyanosis, acrocyanosis, and mild respiratory distress. She was started on supplemental oxygen without improvement. Arterial blood gas demonstrated a PaO2 of 89mmHg and concurrent methemoglobinemia concentration of 18%. She was subsequently given methylene blue 1mg/kg IV with rapid temporal improvement of symptoms. Approximately 4-hours post treatment, her methemoglobin concentration improved to 2%. She was admitted overnight for observation given the long half-life of dapsone and risk of rebound methemoglobinemia; she was discharged the following day with resolution of her symptoms.
Discussion
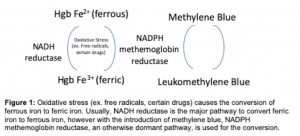
The methemoglobin system can be thought of more as a physiologic mechanism than true pathology. As humans are constantly being bombarded with oxygen free radicals, ferrous 2+ iron offers an electron to make ferric 3+ iron, and then is immediately reduced back to ferrous 2+ iron by methemoglobin reductase, thereby preventing further oxidative stress, including hemolytic anemia and cell membrane lysis (see figure 1). Methemoglobinemia occurs when NADH methemoglobin reductase is overwhelmed and unable to keep up with the oxidative stress and ferric iron is reduced less efficiently. Ferric iron induces a conformational change not only in the hemoglobin that it is attached to, but to the hemoglobin around it, thereby decreasing the oxygen carrying capacity of the hemoglobin units and erythrocytes in general. Cyanosis is more apparent with methemoglobinemia than with de-oxyhemoglobinemia. Perioral cyanosis and palmar cyanosis are usually seen when methemoglobin exceeds 1.5 g/dL, equivalent to 8 to 12 percent methemoglobin at normal hemoglobin concentrations. Common causative agents include benzocaine, dapsone, nitroglycerin, nitrofurantoin, nitroprusside, phenazopyridine, sodium nitrite, amyl nitrate, and isobutyl nitrite.
The treatment for symptomatic methemoglobinemia is methylene blue which is metabolized to leukomethylene blue. This compound increases the activity of NADPH methemoglobin reductase, a minor enzymatic pathway normally (note: this is different that the main NADH methemoglobin reductase), which then reduces ferric iron back to ferrous iron. High dose vitamin C (ascorbic acid) has fallen out of favor due to its inability to rapidly reduce methemoglobin. Following administration of methylene blue, the pulse oximetry usually falls despite clinical improvement as methylene blue further darkens the serum, interfering with the colorimetric assay measuring the percentage of oxygen bound to hemoglobin. Methylene blue should be avoided in cases of patients with G6PD deficiency as this prevents formation of leukomethylene; paradoxically methylene blue (the parent compound) is a potent oxidizing agent and can worsen the oxidative burden. Consequently, methylene blue should be reserved for symptomatic patients. In severe cases, or patients with G6PD deficiency, plasma exchange may be the only option.
Dapsone itself can be difficult to treat as the oxidative cause of methemoglobinemia. Its active metabolite is the major etiology of oxidative stress and has a half-life ranging from 10-50 hours (significantly longer than the half-life of methylene blue ~24 hours). Previous case reports have argued for the utilization of cimetidine following methylene blue to prevent further CYP metabolism of dapsone into its metabolite.
Conclusion:
Clinicians should consider methemoglobinemia in patients whose hypoxia does not readily improved with supplemental oxygen and should review their medication list for common causes of oxidative stress. Be aware of the potential for rebound methemoglobinemia with dapsone due to its long half-life.
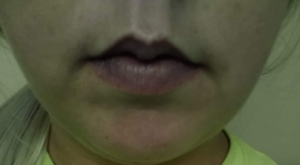
Image 1: Prior to receiving methylene blue

Image 2: 10 minutes after receiving methylene
© permission has been obtained from the UAB Department of Toxicology for use of these images, graphic, and case report.
