Taylor Payne MD
Department of Emergency Medicine, University of Alabama at Birmingham
Introduction
Aortic dissection is a dangerous and easily missed diagnosis. There are many reports of the addition of bedside point-of-care ultrasound to the ED physician’s armamentarium as a rapid way of assessing the patient’s aorta in time-sensitive scenarios. The gold standard for identification of aortic dissection is CT angiography of the chest and abdomen. However, this can be time consuming as it sometimes takes valuable minutes to coordinate staffing and patient transportation to and from the CT scanner. Also, these patients can become rapidly unstable making it less than ideal to remove them from critical care treatment areas. Type A Aortic dissection has a devastating mortality profile with a mortality rate of 1% every hour that the dissection does not get surgical correction.(1) Point-of-care ultrasound has become widely used to evaluate for aortic aneurysm and has more recently become utilized for evaluating aortic dissection.(2,3) There have also been some case studies demonstrating specifically the suprasternal view to visualize the aortic arch to evaluate for dissection.(4,5) This case below demonstrates this technique and shows the images that we acquired on a patient presenting with a known aortic dissection.
Case
A 52-year-old female with a past medical history of hypertension, hyperlipidemia, epilepsy and stroke with left-sided deficits presented to the emergency department with a chief complaint of intermittent chest pain for the last two weeks. She described her chest pain as substernal and pressure-like. The pain was worse with exertion but not improved with rest. She had recently presented to another local hospital and was diagnosed with aortic dissection but was unclear about recommended management. After obtaining this brief history the physician performed a bedside point-of-care ultrasound (POCUS) demonstrating an aortic dissection with a mobile intimal flap. (Image 1) To better visualize the location and extent of the dissection, a suprasternal notch view was obtained with the phased array transducer which demonstrated the dissection into the upper aortic arch. (Image 2) The patient underwent an urgent CT angiography of her chest which visualized a large Stanford type B dissection with severe narrowing of the true lumen. At this time vascular surgery as well as cardiovascular surgery was consulted, and the patient was started on impulse control blood pressure management with esmolol and Clevidipine. The patient subsequently was admitted to the hospital and was discharged after BP, pain control and repeat CTs showing stable dissection. She was admitted 3 weeks later for ongoing chest pain and after unsuccessful attempts at IV blood pressure control underwent and a thoracic endovascular aortic repair (TEVAR) combined with a subclavian-carotid bypass. She was discharged from the hospital two weeks later after successful rehab and was pain free.
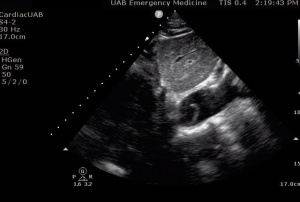
Image 1. Phased Array Transducer longitudinal view along the abdominal Aorta in the sub-xyphoid area. The aorta can be identified by the thick walls and pulsatile nature. See link to video below. The intimal flap was noted to be freely mobile within the aortic lumen.
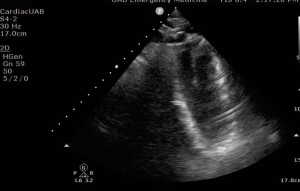
Image 2. Suprasternal notch view of the aortic arch using the phased array transducer. Here we are looking longitudinally down the descending aortic arch with the probe pointing inferiorly. Fanning through transversely will show the entire arch in this view. (not shown) See video below for demonstration of intimal flap motion.

Image 3. Type B Aortic Dissection Seen on CT angiography of the chest in coronal view.
POCUS (point-of-care ultrasound) is an ideal screening tool for rapid assessment of the critically unstable patient in which aortic dissection is being considered. Ultrasound confers no radiation, can quickly be performed at the bedside, and can rule-out some acutely dangerous conditions such as pericardial tamponade. Ultrasonography for aortic dissection is not as sensitive as CT imaging but is moderately specific when a dissection flap is visualized such as in this case. There are few studies looking specifically at the suprasternal notch view and broad analysis of the performance of this view is lacking; however, the consensus with limited data and experience is that this view is preferred when evaluating for dissection. Type B dissections can be more difficult to visualize with the suprasternal view; however, dissection flaps can still be viewed as with this case. The suprasternal view is a fairly novel technique and as more clinicians become comfortable using this technique, it will likely see broader implementation.
References
1. Coady MA, Rizzo JA, Goldstein LJ, Elefteriades JA (1999) Natural history, pathogenesis, and etiology of thoracic aortic aneurysms and dissections. Cardiol Clin 17(4):615–635
2. Goldstein SA, Lindsay J Jr, Vasan R. The diagnosis of thoracic aortic dissection by noninvasive imaging procedures. N Engl J Med. 1993 Jun 3;328(22):1637-8. PubMed PMID: 8487807.
3. Nazerian P, Vanni S, Castelli M, Morello F, Tozzetti C, Zagli G, Giannazzo G, Vergara R, Grifoni S. Diagnostic performance of emergency transthoracic focus cardiac ultrasound in suspected acute type A aortic dissection. Intern Emerg Med. 2014 Sep;9(6):665-70. doi: 10.1007/s11739-014-1080-9. Epub 2014 May 29. PubMed PMID: 24871637.
4. Rosenberg H, Al-Rajhi K. ED ultrasound diagnosis of a type B aortic dissection using the suprasternal view. Am J Emerg Med. 2012 Nov;30(9):2084.e1-5. doi: 10.1016/j.ajem.2011.11.012. Epub 2012 Jan 12. PubMed PMID: 22244228.
5. Fernando SM, Kisilewicz M, Millington SJ. View From the Top: Point-of-Care Ultrasound Diagnosis of Type A Aortic Dissection Using the Suprasternal View. J Emerg Med. 2018 Jan;54(1):e13-e14. doi: 10.1016/j.jemermed.2017.09.019. Epub 2017 Oct 27. PubMed PMID: 29110983.
Copyright permission has been obtained from the UAB Department of Emergency Medicine Division of Ultrasound, Dr. David C. Pigott MD Co-Director of UAB EM Emergency Ultrasound
