Turner, Hannah MD(1); Shufflebarger, Erin MD(1); Rushton, William MD(1,2)
1. Department of Emergency Medicine, University of Alabama-Birmingham
2. Office of Medical Toxicology, University of Alabama-Birmingham
Background:
Paramethoxyamphetamine (PMA) is a potent central nervous system stimulant that can be inadvertently ingested during attempted ingestion of 3,4-methylenedioxymethamphetamine (MDMA). PMA is known to cause severe multi-system organ failure and hyperthermia secondary to uncoupling of oxidative phosphorylation.
Case:
A 15-year-old healthy female was transported to the emergency department for altered mental status after she was found at a friend’s house running around naked. In route to the hospital, she became minimally responsive and vital signs upon arrival were notable for a pulse of 188 beats/min, oral temperature 107 °F (41.6°C), blood pressure 85/30 mmHg, and oxygen saturation 90% on room air. On exam, she was weakly following commands, pupils were approximately 4mm bilaterally, and there was no clonus. Point-of-care glucose revealed mild hypoglycemia at 58mg/dL. She was given 2mg naloxone and 12.5gm of 50% dextrose without improvement in mental status. She had an episode of supraventricular tachycardia, which aborted following parenteral 6mg adenosine. She was subsequently intubated, cold fluid gastric lavage was commenced, and was transferred to the pediatric intensive care unit on Propofol for sedation.
Laboratory evaluation was remarkable for a urine drug screen (UDS) positive for amphetamines, methamphetamines, and cocaine. She also had evidence of elevated alanine aminotransferase peaking at 1424 U/L, aspartate aminotransferase at >4000 U/L, INR 1.7, creatinine 1.15 mg/dL, and rhabdomyolysis with creatinine kinase peaking at 309,427 U/L. Computed tomography head did not demonstrate any evidence of acute intracranial abnormality.
She was extubated shortly after arrival to the ICU but remained very encephalopathic, tachycardic, and agitated. Her agitation responded to intermittent treatment with benzodiazepines. She returned to baseline mental status on hospital day 3 with eventual resolution of her multisystem organ failure.
Discussion:
This case is notable for a patient who presented with severe sympathomimetic toxidrome, as evidenced by cardiac excitability leading to tachydysrhythmia, agitation, mydriasis, and rhabdomyolysis following suspected ingestion. Her presentation is highly suspicious for ingestion of PMA due to her severe hyperthermia and multi-system organ failure, particularly since her UDS was positive for amphetamines. PMA, an amphetamine salt similar to MDMA, can be an inadvertent byproduct in MDMA synthesis. PMA can induce severe hyperthermia and organ failure secondary to uncoupling of oxidative phosphorylation. In normal oxidative phosphorylation, electrons are transferred in the electron transport chain, releasing energy with each transfer. This energy is used to pump protons across the mitochondrial membrane to establish a proton gradient, and ATP synthase uses the energy of the proton gradient to synthesize ATP. Uncouplers, like PMA, reduce the permeability of the mitochondrial membrane and destroy the gradient, allowing energy released by electrons to form heat rather than ATP, inducing hyperthermia (see figure 1). Multiple case reports have documented instances of PMA ingestions in which hyperthermia and multi-system organ failure were ultimately fatal. The mainstay of treatment is aggressive cooling and deep sedation to stabilize the sympathetic nervous system.
Conclusion:
Severe hyperthermia and multi-system organ failure in the setting of amphetamine ingestion should prompt the clinician to consider uncoupling of oxidative phosphorylation as a mechanism of hyperthermia, particularly when considering inadvertent ingestion of PMA. Under such circumstances, practitioners should consider deep sedation and aggressive cooling measures.
See also:
- Becker J, Neis P, Röhrich J, Zörntlein S. A fatal paramethoxymethamphetamine intoxication. Legal Medicine. 2003 Mar 1;5:S138-41.
- Shin EJ, Dang DK, Tran HQ, Nam Y, Jeong JH, Lee YH, Park KT, Lee YS, Jang CG, Hong JS, Nabeshima T. PKCδ knockout mice are protected from para-methoxymethamphetamine-induced mitochondrial stress and associated neurotoxicity in the striatum of mice. Neurochemistry international. 2016 Nov 1;100:146-58.
- Nicol JJ, Yarema MC, Jones GR, Martz W, Purssell RA, MacDonald JC, Wishart I, Durigon M, Tzemis D, Buxton JA. Deaths from exposure to paramethoxymethamphetamine in Alberta and British Columbia, Canada: a case series. CMAJ open. 2015 Jan;3(1):E83.
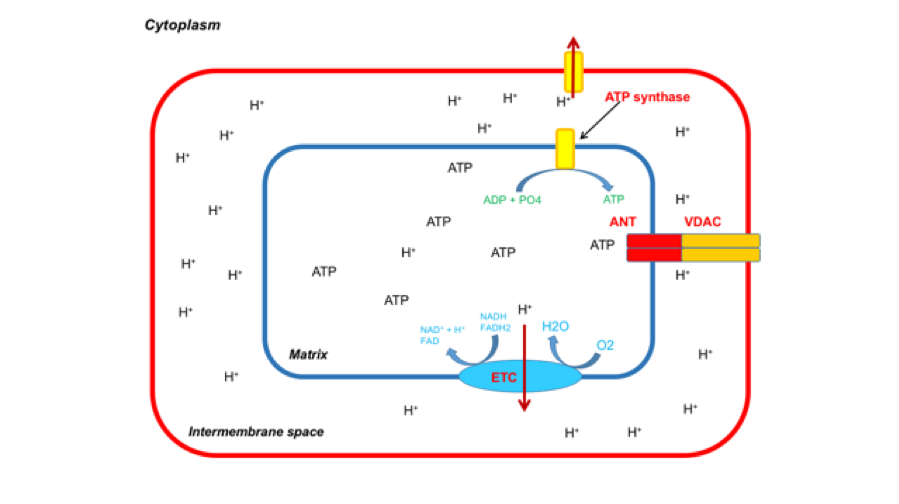
Figure 1: Normal physiology of the mitochondrial where hydrogen ions are pumped by the electron transport chain into the intermembrane space, which then comes back into the mitochondrial matrix forming ATP.
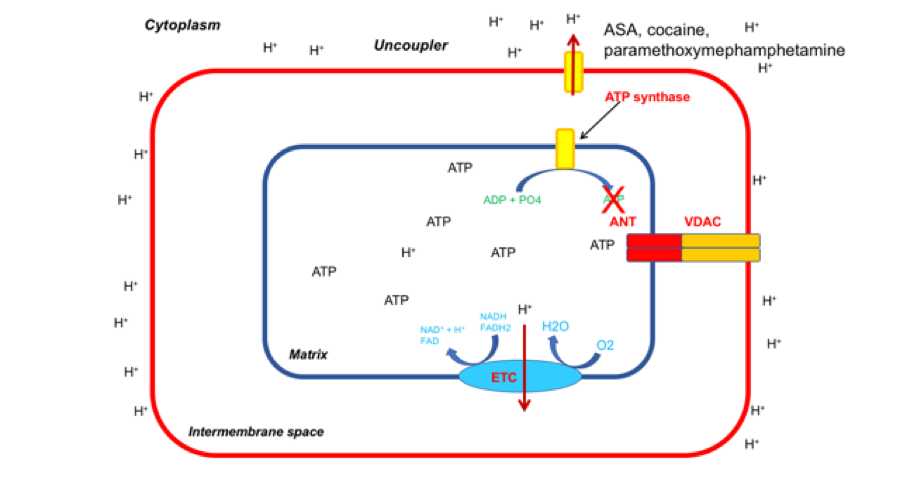
Figure 2: In the presence of an uncoupler like paramethoxymephamphetamine, a channel opens from the intermembrane mitochondrial space into the surrounding cytoplasm, allowing hydrogen ions to diffuse out of the mitochondria, disrupting the hydrogen ion gradient. This limits production of ATP; energy formed by the electron transport chain is released as entropy leading to the severe hyperthermia seen in uncoupling physiology.
